Preventing treatment inertia: 2020 ACR Guidelines discuss that ULT titration should occur over weeks to months, not years3
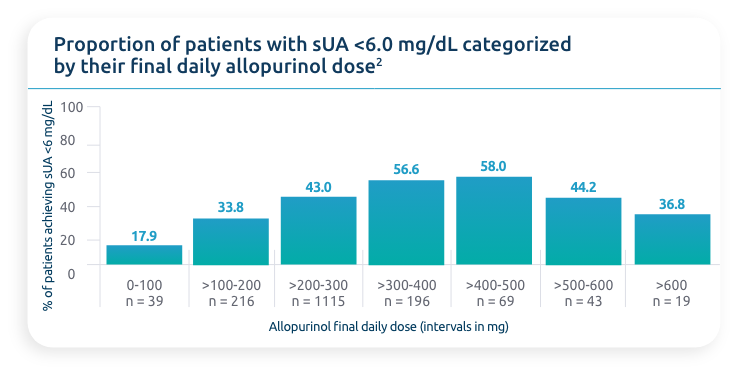
Uptitrating oral ULTs oftentimes yields diminishing returns1
This can be explained in 2 ways:
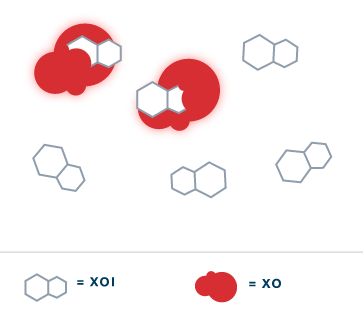
Enzyme Limitations
- Once xanthine oxidase (XO) in the body has been saturated, increasing the dose of xanthine oxidase inhibitors (XOIs) is unlikely to have any additional effect on uric acid metabolism4
Existing Burden
- While XOIs can limit the production of uric acid, they do not actively remove saturated urate from the body4
- XOIs, by their mechanism, do not actively address uric acid that has already been produced4
sUA, serum uric acid; ULT, urate-lowering therapy.

